MANAGEMENT OF CHRONIC VENTILATORY FAILURE IN ADVANCED-STAGE NEUROMUSCULAR DISORDERS
ABSTRACT:
Chronic ventilatory failure is a major cause of morbidity and mortality among patients affected with neuromuscular disorders. Although evidence from controlled trials is lacking, administration of long-term non-invasive ventilatory supporwt appears to improve physiologic parameters, the quality of life and life-expectancy. The main indications for non-invasive mechanical ventilation are deteriorating symptoms of hypercapnia, abnormalities in blood gases either during sleep or wakefulness, and a severe decrease in lung volume for rapidly progressive disease.
INTRODUCTION
Insidious, late-onset ventilatory failure is a major cause of morbidity and mortality among patients affected with various kinds of Neuromuscular Disorders (NMD) (see table I). Nevertheless, the treatment of neuromuscular respiratory failure was for many years considered to be “most controversial” and “to raise enormous ethical difficulties” due to the lack of effective therapeutic approaches and to the severely impaired quality of life of neuromyopathic patients at an advanced stage of disease (1) (Table 1).
The proven success of long-term mechanical ventilation administered invasively by an indwelling tracheostomy tube (IMV) in prolonging survival of such patients has not had a substantial impact on this problem, the most frequently cited reason being a lack of improvement in the patient’s and family’s quality of life. In fact, IMV often restricts the user’s lifestyle, requiring a high level of care, and frequently obliges the patient’s family to sacrifice personal time and privacy, thus exacerbating depression and anxiety (2).
However, in recent years the approach to care of neuromuscular respiratory failure by long-term mechanical ventilation has been revised, due to two new critical developments:
-technology has advanced and several new types of ventilatory aids have been introduced, which deliver effective mechanical ventilation even non-invasively, by way of a nasal mask or a mouthpiece; non-invasive ventilation is characterized by ease of administration, preservation of upper airway function and lower cost.
-the majority of severely disabled ventilator users with neuromuscular disease have expressed satisfaction with their lives, even though they are usually unable to achieve some of the goals associated with acceptable quality of life in the “normal” population (3).
As a consequence, and thanks to an ethos of optimism, increasing numbers of neuromyopathic patients with advanced respiratory impairment are now being successfully treated by long-term Non-Invasive Mechanical Ventilation (NIV), usually in the home setting.
LONG-TERM NON-INVASIVE MECHANICAL VENTILATION (NIV)
MODES OF VENTILATION
Both negative pressure devices (i.e., iron lung, cruirass, wrap ventilator) and positive pressure ventilators have been used successfully in the non-invasive management of chronic ventilatory failure related to neuromuscular disorders; however, since the mid-1980s, Positive Pressure Ventilation (PPV) has become the most widespread technique, mostly due to the availability of comfortable nasal interfaces and increased practitioner experience.
The non-invasive administration of PPV requires a positive pressure ventilator delivering pressurized gas to the lungs through an interface with the nose or mouth or both; the expired gas is conducted away from the patient without contaminating the inspired gas, except in the dead space of the circuit close to the patient.
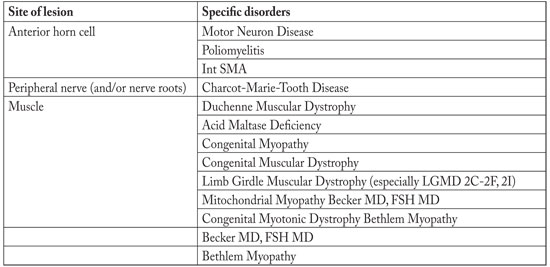
Table 1. Neuromuscular Disorders which are likely to cause chronic ventilatory failure.
While the earliest ventilators used for Non-Invasive Positive Pressure Ventilation (NPPV) were unsophisticated volume-limited devices, in recent years manufacturers have developed a new generation of microprocessor-controlled ventilators that supply both volume- and pressure-limited modes and have special features designed to facilitate the application of non-invasive techniques. They are generally simple, reliable and easy for the patient to use (4).
There is no consensus on the optimal interface to use in delivering NPPV: commercially available mask interfaces include nasal masks, nasal pillows or plugs, mouthpieces, full-face (oronasal) masks and custommade nasal masks. Nasal masks are usually preferable for nocturnal ventilation, due to the fact that they are more comfortable and permit better speech (fig.1); on the other hand, oronasal interfaces may be a suitable alternative for subjects who have excessive air leaking through the mouth or nose. Mouthpiece interfaces have also been successfully used to deliver NPPV for up to 24h/day (5).
Finally, the choice of ventilator and interface in most cases is individualized according to patients’ preference and physicians’ intuition and experience, rather than based on standardized evidence-based guidelines.

Figure 1. Nasal mask for nocturnal ventilation
Application of Non-Invasive Positive Pressure Ventilation by a nasal mask on a young patient with Neuromuscular Disease.
INDICATIONS
Long-term NIV is required when spontaneous respiratory muscle efforts are unable to sustain adequate alveolar ventilation, causing chronic stable or slowly progressive ventilatory failure. If reversible deteriorating factors (i.e., respiratory infection, congestive heart failure, severe electrolyte disturbance, etc.) have been treated successfully, indications for NIV are defined by the following, persisting conditions (6):
1. Symptoms attributable to hypoventilation (such as fatigue, dyspnea, morning headache) and one of the following:
2. Physiologic criteria:
-Significant daytime CO2 retention (PaCO2 > 50 mmHg);
-Nocturnal oxygen desaturation (SaO2 < 88% for at least five consecutive minutes);
-Forced Vital Capacity < 50% predicted or Maximal Inspiratory Pressure < 60 cm H2O, only for rapidly progressive disease.
The following complications are considered to be contraindications for NIV:
1. severely impaired swallowing, leading to chronic aspiration and repeated pneumonia;
2. ineffective clearing of tracheobronchial secretions, despite the use of non-invasive manual or mechanical expiratory aids;
3. need for round-the-clock (>20h) ventilator support.
These are conditions usually requiring an invasive application of MV. It should be noted that the combination of NPPV with assisted coughing techniques or crycothyroid “minitracheostomy” may avoid tracheostomy- PPV in subjects with severe inability to cough out airway secretions (7-9).
NIV is sometimes technically difficult to apply, especially in infants and young children, and requires motivation and cooperation on the part of the patient. If non-invasive techniques are not well-tolerated or unsuccessful, a tracheostomy could be performed electively, before the patient has developed major complications of chronic ventilatory insufficiency. Possible causes of failure of NIV and management strategy are reported in table 2.
MECHANISM OF ACTION
Although there is general agreement that the administration of nocturnal PPV to neuromyopathic patients with chronic hypoventilation results in increased daytime spontaneous ventilation (10), there is less consensus regarding the mechanisms by which diurnal symptoms and arterial blood gases (ABG) are improved by night-time PPV. Three theories have been proposed to explain these beneficial effects. According to the “lung mechanics hypothesis”, positive pressure ventilation acts by improving the derangement in respiratory mechanics, decreasing stiffness of the respiratory system and reducing the elastic effort of breathing; this theory is based on the observation that short-term administration of PPV may induce an increase in lung compliance and Functional Residual Capacity; however, it requires further investigations (11).

Table 2. Causes of failure of Non-Invasive Positive Pressure Ventilation and management strategy (VT = Tidal Volume).
The “rest hypothesis” proposes that nocturnal ventilation rests chronically fatigued ventilator muscles, thereby improving daytime ventilatory performance and ABG; this theory has been confirmed by the finding of reduced EMG activity of the diaphragm and esophageal pressure swings in patients with chronic hypoventilation during non-invasive PPV (12); however, the relation between muscle fatigue and chronic respiratory failure is not evident (13). And finally, the “set point hypothesis” argues that, by reducing nocturnal CO2 retention, night-time assisted ventilation reverses “central fatigue”, improves respiratory sensitivity and lowers the CO2 set-point; as a consequence, daytime ventilation tends to improve progressively. Supportive evidence for this theory derives from studies demonstrating that the reduction in PaCO2 observed after nocturnal PPV correlates with the increase in the slope of the ventilatory response to the CO2 curve, although respiratory muscle strength remains unchanged (14,15).
RESULTS
Administration of NIV to neuromyopathic patients with chronic hypoventilation may be expected to improve physiologic function and quality of life as well as decrease the frequency of episodes requiring acute care facilities. In particular:
-Physiological indices: although physiological outcomes of NPPV remain conflicting in DMD patients, Maximum Inspiratory Pressure and Vital Capacity may transiently increase or stabilize (16,17). Night-time (direct effect) and daytime (indirect effect) ABG values tend to normalize promptly after initiation of NPPV (18);
-Pulmonary morbidity: NIV decreases the risk of respiratory complications and hospitalizations and postpones the last-resort necessity of performing a tracheostomy by months to years, depending on the rate of progression of bulbar muscle dysfunction (19,20);
-Quality of life: NPPV users usually report an alleviation of symptoms related to CO2 retention; in addition, they have been proven to be comparable to other age-matched groups in terms of health perception and social integration (3,21);
-Survival: NPPV has been demonstrated to prolong life in Duchenne’s Muscular Dystrophy (DMD), the mean survival in hypercapnic DMD patients without ventilatory support being only 9.7 months (22). In DMD patients, NPPV is generally considered to provide an additional life’s expectancy of 5–10 years (23,24).
Although restricted to uncontrolled series of patients due to obvious ethical reasons, the results of our experience suggest that the administration of NPPV in DMD may not only increase survival, but also have a dramatic impact on the causes of death. In fact, whilst unventilated DMD patients have been reported die as a result of respiratory insufficiency in 70% of cases (25), the great majority of our patients submitted to long-term ventilatory treatment die of a cardiopathy: as a final effect, the natural history of the disease is significantly changed.
CONCLUSIONS
The long-term use of NIV can alleviate symptoms for neuromyopathic patients with chronic ventilator failure; it can avoid tracheostomy, and can prolong survival for some patients. The effects of NIV are almost certainly multifactorial and further studies are necessary to clarify the most important mechanisms of action, and thereby facilitate more rational use.
BIBLIOGRAPHY
- Smith PEM, Calverley PMA, Edwards RHT et al. Practical problems in the respiratory care of individuals with muscular dystrophy. N Engl J Med 1987; 316: 1197-204
- Moss AH, Oppenheimer EA, Casey P, Cazzolli PA, Roos RP, Stocking CB, Siegler M. Patients With Amyotrophic Lateral Sclerosis Receiving Long-term Mechanical Ventilation: Advance Care Planning and Outcomes. Chest 1996;110;249-55
- Kohler M,. Clarenbach CF, Böni L, et al. Quality of Life, Physical Disability, and Respiratory Impairment in Duchenne Muscular Dystrophy. Am J Respir Crit Care Med 2005; 172: 1032-6
- Fauroux B, Leroux K, Pépin JL, et al. Are home ventilators able to guarantee a minimal tidal volume? Intensive Care Med 2010; 36: 1008-14.
- Hess DR. Noninvasive ventilation in neuromuscular disease: equipment and application. Respir. Care 2006 ; 51: 896-911
- Consensus Conference. Clinical indications for noninvasive positive pressure ventilation in chronic respiratory failure due to restrictive lung disease, COPD and nocturnal hypoventilation. A Consensus Conference report. Chest 1999; 116: 521-34
- Vianello A, Bevilacqua M, Arcaro G, Serra E. Prevention of pulmonary morbidity in patients with neuromuscular disorders. A possible role for permanent cricothyroid “minitracheostomy”. Chest 1998; 114: 346-7
- Gomez‑Merino E, Bach JR. Duchenne muscular dystrophy: prolongation of life by noninvasive respiratory muscle aids. Am J Phys Med Rehabil 2002;81:411‑5.
- Vianello A, Corrado A, Arcaro G, Gallan F, Ori C, Minuzzo M, Bevilacqua M. Mechanical Insufflation-Exsufflation improves outcomes for neuromuscular disease patients with respiratory tract infections. Am J Phys Med Rehabil 2005;84:83-8
- Simonds A, Muntoni F, Heather S, et al. Impact of nasal ventilation on survival in hypercapnic Duchenne muscular dystrophy. Thorax 1998; 53: 949-52
- McCool FD, Mayewski RF, Shayne DS et al. Intermittent positive pressure breathing in patients with respiratory muscle weakness. Alterations in total respiratory system compliance. Chest 1986; 90: 546–52.
- Carrey Z, Gottfried SB, Levy RD. Ventilatory muscle support in respiratory failure with nasal positive pressure ventilation. Chest 1990; 97: 150-8
- Vassilakopoulos T, Zakynthinos S, Roussos C. Bench-tobedside review: Weaning failure: should we rest the respiratory muscles with controlled mechanical ventilation? Crit Care 2006; 10: 204-8
- Annane D, Quera-Salva MA, Lofaso F et al. Mechanisms underlying effects of nocturnal ventilation on daytime blood gases in neuromuscular diseases. Eur Respir J 1999;13: 157-62
- Nickol AH, Hart N, Hopkinson NS et al. Mechanisms of improvement of respiratory failure in patients with restrictive thoracic disease treated with non-invasive ventilation. Thorax 2005; 60: 754–60.
- Goldstein RS, DeRosie JA, Avendano MA, Dolmage TE. Influence of non-invasive positive pressure ventilation on inspiratory muscles. Chest 1991; 99: 408-15
- Benditt JO. Full-time noninvasive ventilation: possible and desirable. Respir Care 2006; 51: 1005–12
- Annane D, Chevrolet JC, Chevret S et al. Nocturnal mechanical ventilation for chronic hypoventilation in patients with neuromuscular and chest wall disorders. Cochrane Database Syst Rev 2000; CD001941
- Leger P, Bedicam JM, Conette A et al. Nasal Intermittent Positive Pressure Ventilation. Long-term follow-up in patients with svere chronic respiratory insufficiency. Chest 1994; 105: 100-5
- Katz S, Selvadurai H, Keilty K et al. Outcome of non-invasive positive pressure ventilation in paediatric neuromuscular disease. Arch Dis Child 2004; 89: 121–4
- Simonds AK. Neuromuscular disorders. In: Muir JF, Ambrosino N, Simonds AK, eds. Noninvasive mechanical ventilation. Sheffield, European Respiratory Society Journal Ltd, 2001; pp 218-26
- Vianello A, Bevilacqua M, Salvador V, Cardaioli C, Vincenti E. Long-term nasal intermittent positive pressure ventilation in advanced Duchenne’s Muscular Dystrophy. Chest 1994; 105: 445-8
- Eagle M, Baudouin SV, Chandler C, et al. Survival in Duchenne muscular dystrophy: improvements in life expectancy since 1967 and the impact of home nocturnal ventilation. Neuromuscul Disord 2002;12:926–9
- Jeppesen J, Green A, Steffensen BF et al. The Duchenne muscular dystrophy population in Denmark, 1977–2001: prevalence, incidence and survival in relation to the introduction of ventilator use. Neuromuscul Disord 2003; 13: 804–12
- Rideau Y, Gatin G, Bach J et al. Prolongation of life in Duchenne’s muscular dystrophy. Acta Neurol 1983; 5: 118–24.
Correspondence to:
Andrea Vianello, MD, U.O. Fisiopatologia Respiratoria, Azienda Ospedaliera di Padova, Via Giustiniani, 2, 35128 PADOVA – Italy, Phone: 0039-049-8218587, Fax: 0039-049-8218590, avianello@qubisoft.it

